Engineering primary T cells with chimeric antigen receptors for rewired responses to soluble ligands
The expression of synthetic receptors in primary T cells enables the programming of user-defined responses when designing T-cell therapies. Chimeric antigen receptors (CARs) are synthetic receptors that have demonstrated efficacy in cancer therapy by targeting immobilized antigens on the surface of malignant cells. Recently, we showed they can also rewire T-cell responses to soluble ligands. In contrast to other synthetic receptors, CARs are not only readily engineered by rational design, but also clinically translatable, with robust function in primary human T cells. This protocol discusses design principles for CARs responsive to soluble ligands and delineates steps for producing T cells expressing synthetic receptors. Functional assays for quantifying the ability of CAR T cells to sense and respond to soluble ligands are also presented. This protocol provides a framework for proficient immune-cell researchers to test novel T-cell therapies targeting soluble ligands in
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
265,23 € per year
only 22,10 € per issue
Buy this article
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others

Engineering strategies to overcome the current roadblocks in CAR T cell therapy
Article 17 December 2019

CTLA-4 tail fusion enhances CAR-T antitumor immunity
Article 27 July 2023

HLA-independent T cell receptors for targeting tumors with low antigen density
Article 13 January 2022
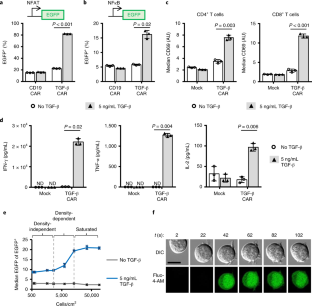
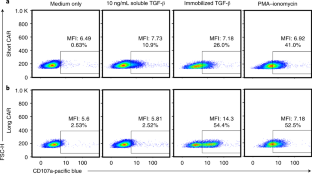
Data availability
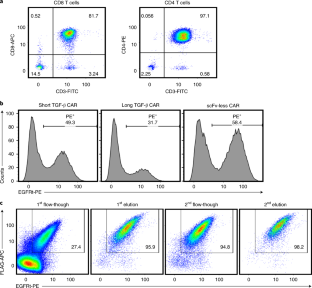
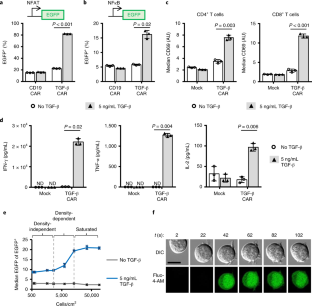
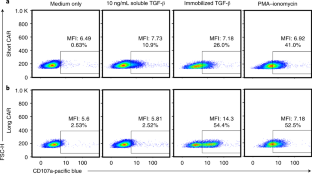
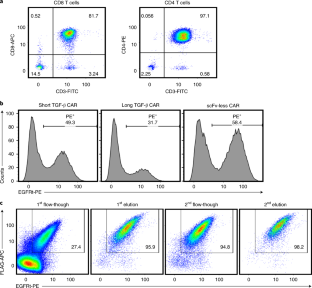
The data analyzed to generate what is shown in this manuscript are compiled in the Supplementary Spreadsheet file. Individual examples of gating strategy are shown when appropriate. Data from Fig. 4 and Supplementary Fig. 3 have been used in a prior publication 6 .
References
- Maude, S. L. et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N. Engl. J. Med.371, 1507–1517 (2014). ArticleGoogle Scholar
- Maude, S. L. et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N. Engl. J. Med.378, 439–448 (2018). ArticleCASGoogle Scholar
- Porter, D. L. et al. Chimeric antigen receptor T cells persist and induce sustained remissions in relapsed refractory chronic lymphocytic leukemia. Sci. Transl. Med.7, 303ra139 (2015). ArticleGoogle Scholar
- Brentjens, R. J. et al. Safety and persistence of adoptively transferred autologous CD19-targeted T cells in patients with relapsed or chemotherapy refractory B-cell leukemias. Blood118, 4817–4828 (2011). ArticleCASGoogle Scholar
- Kochenderfer, J. N. et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J. Clin. Oncol.33, 540–549 (2015). ArticleCASGoogle Scholar
- Chang, Z. L. et al. Rewiring T-cell responses to soluble factors with chimeric antigen receptors. Nat. Chem. Biol.14, 317–324 (2018). ArticleCASGoogle Scholar
- Hou, A. J., Chang, Z. L., Lorenzini, M. H., Zah, E. & Chen, Y. Y. TGF‐β–responsive CAR‐T cells promote anti‐tumor immune function. Bioeng. Transl. Med3, 75–86 (2018). ArticleCASGoogle Scholar
- Chen, L. C. & Chen, Y. Y. Outsmarting and outmuscling cancer cells with synthetic and systems immunology. Curr. Opin. Biotechnol.60, 111–118 (2019). ArticleCASGoogle Scholar
- Leen, A. M. et al. Reversal of tumor immune inhibition using a chimeric cytokine receptor. Mol. Ther.22, 1211–1220 (2014). ArticleCASGoogle Scholar
- Mohammed, S. et al. Improving chimeric antigen receptor-modified T cell function by reversing the immunosuppressive tumor microenvironment of pancreatic cancer. Mol. Ther.25, 249–258 (2017). ArticleCASGoogle Scholar
- Wilkie, S. et al. Selective expansion of chimeric antigen receptor-targeted T-cells with potent effector function using interleukin-4. J. Biol. Chem.285, 25538–25544 (2010). ArticleCASGoogle Scholar
- Chang, Z. L. & Chen, Y. Y. CARs: synthetic immunoreceptors for cancer therapy and beyond. Trends Mol. Med.23, 430–450 (2017). ArticleCASGoogle Scholar
- Schwarz, K. A., Daringer, N. M., Dolberg, T. B. & Leonard, J. N. Rewiring human cellular input-output using modular extracellular sensors. Nat. Chem. Biol.13, 202–209 (2017). ArticleCASGoogle Scholar
- Baeumler, T. A., Ahmed, A. A. & Fulga, T. A. Engineering synthetic signaling pathways with programmable dcas9-based chimeric receptors. Cell Rep.20, 2639–2653 (2017). ArticleCASGoogle Scholar
- Scheller, L., Strittmatter, T., Fuchs, D., Bojar, D. & Fussenegger, M. Generalized extracellular molecule sensor platform for programming cellular behavior. Nat. Chem. Biol.14, 723 (2018). ArticleCASGoogle Scholar
- Green, M. R. & Sambrook, J. Molecular Cloning: A Laboratory Manual (Cold Spring Harbor Press, 2012).
- Gibson, D. G. et al. Enzymatic assembly of DNA molecules up to several hundred kilobases. Nat. Methods6, 343–345 (2009). ArticleCASGoogle Scholar
- Tiscornia, G., Singer, O. & Verma, I. M. Production and purification of lentiviral vectors. Nat. Protoc.1, 241–245 (2006). ArticleCASGoogle Scholar
- Liu, L. et al. Inclusion of Strep-tag II in design of antigen receptors for T-cell immunotherapy. Nat. Biotechnol.34, 430–434 (2016). ArticleCASGoogle Scholar
- Ghassemi, S. et al. Reducing ex vivo culture improves the antileukemic activity of chimeric antigen receptor (CAR) T cells. Cancer Immunol. Res.6, 1100–1109 (2018). ArticleCASGoogle Scholar
- Hollyman, D. et al. Manufacturing validation of biologically functional T cells targeted to CD19 antigen for autologous adoptive cell therapy. J. Immunother.32, 169–180 (2009). ArticleCASGoogle Scholar
- Vormittag, P., Gunn, R., Ghorashian, S. & Veraitch, F. S. A guide to manufacturing CAR T cell therapies. Curr. Opin. Biotechnol.53, 164–181 (2018). ArticleCASGoogle Scholar
- Chang, Z. L. et al. Rewiring T-cell signaling responses to extracellular soluble cues with chimeric antigen receptors. Mol. Ther.27, abstr. 832 (2019). Google Scholar
- Zah, E., Lin, M.-Y., Silva-Benedict, A., Jensen, M. C. & Chen, Y. Y. T cells expressing CD19/CD20 bispecific chimeric antigen receptors prevent antigen escape by malignant B cells. Cancer Immunol. Res.4, 498–508 (2016). ArticleCASGoogle Scholar
- Caruso, H. G. et al. Tuning sensitivity of CAR to EGFR density limits recognition of normal tissue while maintaining potent antitumor activity. Cancer Res.75, 3505–3518 (2015). ArticleCASGoogle Scholar
- Liu, X. et al. Affinity-tuned ErbB2 or EGFR chimeric antigen receptor T cells exhibit an increased therapeutic index against tumors in mice. Cancer Res.75, 3596–3607 (2015). ArticleCASGoogle Scholar
- Wang, X. et al. A transgene-encoded cell surface polypeptide for selection, in vivo tracking, and ablation of engineered cells. Blood118, 1255–1263 (2011). ArticleCASGoogle Scholar
- Wei, P. et al. Bacterial virulence proteins as tools to rewire kinase pathways in yeast and immune cells. Nature488, 384–388 (2012). ArticleCASGoogle Scholar
- Wang, D. et al. A requirement for CARMA1 in TCR-induced NF-κB activation. Nat. Immunol.3, 830–835 (2002). ArticleCASGoogle Scholar
- Long, A. H. et al. 4-1BB costimulation ameliorates T cell exhaustion induced by tonic signaling of chimeric antigen receptors. Nat. Med.21, 581–590 (2015). ArticleCASGoogle Scholar
- Frigault, M. J. et al. Identification of chimeric antigen receptors that mediate constitutive or inducible proliferation of T cells. Cancer Immunol. Res.3, 356–367 (2015). ArticleCASGoogle Scholar
- Aivazian, D. & Stern, L. J. Phosphorylation of T cell receptor ζ is regulated by a lipid dependent folding transition. Nat. Struct. Biol.7, 1023–1026 (2000). ArticleCASGoogle Scholar
- Zhang, H., Cordoba, S.-P., Dushek, O. & van der Merwe, P. A. Basic residues in the T-cell receptor ζ cytoplasmic domain mediate membrane association and modulate signaling. Proc. Natl Acad. Sci. USA108, 19323–19328 (2011). ArticleCASGoogle Scholar
- Dobbins, J. et al. Binding of the cytoplasmic domain of CD28 to the plasma membrane inhibits Lck recruitment and signaling. Sci. Signal.9, ra75–ra75 (2016). ArticleGoogle Scholar
Acknowledgements
Several protocols presented reflect discussion and contributions from present and past members of the Chen lab, notably E. Zah, P. Ho, M.-y. Lin, and M. Lorenzini, as well as members of the M. Jensen lab (Seattle Children’s Research Institute). The NFAT reporter Jurkat T-cell line was a gift from A. Weiss (University of California, San Francisco). The NFκB reporter Jurkat T-cell line was a gift from X. Lin (University of Texas MD Anderson Cancer Center). This work was supported by the National Institutes of Health (grant DP5OD012133, UC CAI grant U54HL119893, and UCLA CTSI grant UL1TR001881 to Y.Y.C.). Z.L.C. was supported by an NIH F30 Fellowship (F30CA183528). A.J.H. was supported by the NIH Biotechnology Training in Biomedical Sciences and Engineering Program (T32 GM067555).
Author information
- ZeNan L. Chang Present address: Department of Medicine, Washington University in St. Louis, St. Louis, MO, USA
- These authors contributed equally: ZeNan L. Chang, Andrew J. Hou.
Authors and Affiliations
- Department of Chemical and Biomolecular Engineering, University of California, Los Angeles (UCLA), Los Angeles, CA, USA ZeNan L. Chang, Andrew J. Hou & Yvonne Y. Chen
- Department of Microbiology, Immunology, and Molecular Genetics, University of California, Los Angeles (UCLA), Los Angeles, CA, USA Yvonne Y. Chen
- Parker Institute for Cancer Immunotherapy Center at UCLA, Los Angeles, CA, USA Yvonne Y. Chen
- ZeNan L. Chang